Implantology
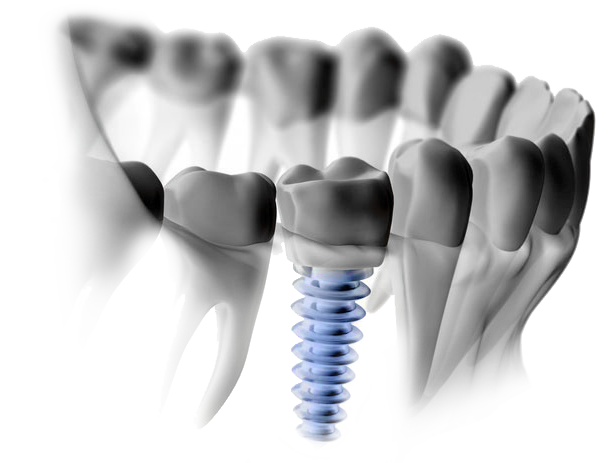
A dental implant is a replacement for the root or roots of a tooth. Like tooth roots, dental implants are secured in the jawbone and are not visible once surgically placed. They are used to secure crowns (the parts of teeth seen in the mouth), bridgework or dentures by a variety of means. They are made of titanium, which is lightweight, strong and biocompatible, which means that it is not rejected by the body. Titanium and titanium alloys are the most widely used metals in both dental and other bone implants, such as orthopedic joint replacements. Dental implants have the highest success rate of any implanted surgical device. Titanium’s special property of fusing to bone, called osseointegration (“osseo” – bone; “integration” – fusion or joining with), is the biological basis of dental implant success. That’s because when teeth are lost, the bone that supported those teeth is lost too. Placing dental implants stabilizes bone, preventing its loss. Along with replacing lost teeth, implants help maintain the jawbone’s shape and density. This means they also support the facial skeleton and, indirectly, the soft tissue structures — gum tissues, cheeks and lips. Dental implants help you eat, chew, smile, talk and look completely natural. This functionality imparts social, psychological and physical well-being.

Am I a candidate for dental implants?
Generally speaking, if you have lost teeth you are a candidate for dental implants. It is important that you are in good health, however, as there are some conditions and diseases that can affect whether dental implants are right for you. For example, uncontrolled diabetes, cancer, radiation to the jaws, smoking, alcoholism, or uncontrolled periodontal (gum) disease may affect whether dental implants will fuse to your bone. It is important to let your dental surgeon know all about your medical status (past and present) together with all medications you are taking, whether prescribed, alternative (herbal) or over-the-counter.Where and how implants are placed requires a detailed assessment of your overall stomato-gnathic system (“stoma” – mouth; “gnathic” – jaws), within which the teeth function. This will necessitate compiling records that include study models of your mouth and bite, and specialized radiographs (x-rays), which may include 3D scans known as computerized tomograms (CT scans). Planning with the help of computer imaging ensures that dental implants can be placed in exactly the right position in the bone.
How and why is bone lost when teeth are lost?
Bone needs stimulation to maintain its form and density. In the case of alveolar (sac-like) bone that surrounds and supports teeth, the necessary stimulation comes from the teeth themselves. When a tooth is lost, the lack of stimulation causes loss of alveolar bone. There is a 25% decrease in width of bone during the first year after tooth loss and an overall decrease in height over the next few years.The more teeth lost, the more function lost. This leads to some particularly serious aesthetic and functional problems, particularly in people who have lost all of their teeth. And it doesn’t stop there. After alveolar bone is lost, the bone beneath it, basal bone — the jawbone proper — also begins to resorb (melt away).




What are the options for implant tooth replacement?
Single Tooth Replacement: Immediately (at the same time an implant is placed) or after a period of healing, an abutment is attached to the implant. This is a device that “abuts” or joins the implant to a tooth form called a crown, which replaces the tooth part you see in the mouth. It will hold a custom-made crown that the dental laboratory will fabricate and match to your existing teeth. The custom crown is cemented or screwed onto the abutment to permanently keep it in place. Once the crown is in place, it should be indistinguishable from your natural teeth.
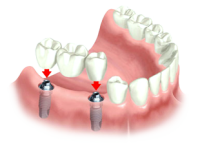
Fixed Multiple Tooth Replacement
As with single tooth replacement, temporary healing caps or abutments may be placed on multiple implants until the healing phase is complete. After healing, permanent abutments are attached to the implants. They can attach to custom-made crowns or bridgework that a dental laboratory will fabricate to match your existing teeth. In the final step, the custom bridge, which will replace multiple teeth, is cemented or screwed onto the abutments. The teeth have been replaced without disturbing the healthy teeth next to them, and bone loss has been halted.
Removable Implant-Supported Tooth Replacement:
If all of your lower teeth are missing, depending on the design of the removable restoration, two to six implants may be used to support a lower denture. If all of your upper teeth are missing, a minimum of four implants may be used to support an upper denture. Removable dentures are often used to replace extensive tooth, bone and gum-tissue loss, thus providing support for the facial skeleton, lip and cheeks. A new denture can have attachments that snap or clip it into place on the implants or a custom made, milled bar can be fabricated to create additional strength and support for the restoration. Design variations are often related to your bone density and number of implants present; your dentist will discuss these options during your consultation. A significant advantage of a removable denture is facilitating the cleaning of the dental implants.
What type of maintenance do dental implants require?
Implant crowns and other prosthetic (false) tooth replacements are made to be remarkably failsafe systems. They are removable and replaceable (only by your dentist), so that if damage or wear necessitates replacement, this can be accomplished without affecting the implant(s) or attachment to the bone. Nevertheless, implants do require maintenance. It is important to practice good daily oral hygiene, including brushing and flossing to control bacterial biofilm. It is also important to see your dentist and dental hygienist. Special instruments are necessary to clean dental implants that will not damage their metal surface beneath the gum tissues. Your dentist will need to monitor your implants to make sure the integrity of the osseointegration is stable, and that the implant crowns, bridgework or dentures are functioning adequately.